When Are Providers Responsible For Obtaining An Abn For A Service Not Considered Medically Necessary
What's Changed?
- Updated resources with a link to the Beneficiary Notices Initiative (BNI) Library webpage
Utilize this educational tool by selecting the tabs above or scrolling to each department.
Using the ABN Tutorial
Select any field (messages A–J) for details on how to consummate each ABN department.
Quick Get-go
The Accelerate Casher Notice of Non-coverage (ABN), Form (CMS-R-131) helps Medicare Fee-for-Service (FFS) beneficiaries brand informed decisions nearly items and services Medicare usually covers merely may not cover in specific situations. For example, the items or services may not be medically necessary for a beneficiary.
Read the total Quick Start
When health care providers and suppliers await a Medicare coverage deprival for a service Medicare generally covers, they must issue an ABN to transfer financial liability to the beneficiary, including:
- Independent labs, Skilled Nursing Facilities (SNFs), and Home Health Agencies (HHAs) providing Medicare Part B (outpatient) items and services
- Hospice providers, HHAs, and Religious Not-Medical Health Care Institutions providing Part A (inpatient) items and services
This educational tool shows health care providers and suppliers how to correctly complete an ABN form. In this ABN tutorial, you refers to the provider or supplier issuing the form. On the ABN form, you refers to the beneficiary signing it.
Close
Requirements
You must upshot an ABN:
- When a Medicare item or service isn't reasonable and necessary under Plan standards, including care that'southward:
- Not indicated for the diagnosis, handling of illness, injury, or to ameliorate the functioning of a malformed body fellow member
- Experimental and investigational or considered research only
- More than than the number of services immune in a specific menses for that diagnosis
Read the full Requirements
- When providing custodial care
- When outpatient therapy services exceed therapy threshold amounts
- Before caring for a beneficiary who isn't terminally ill (hospice providers)
- Before caring for a beneficiary who isn't confined to the home or doesn't need intermittent skilled nursing intendance (home health providers)
- Before providing a preventive service we normally cover but won't cover in specific situations when services exceed frequency limits
- Before providing a Medicare detail or service nosotros won't cover (Durable Medical Equipment, Prosthetics, Orthotics, and Supplies [DMEPOS] suppliers) considering:
- Provider accustomed prohibited unsolicited phone contacts
- Supplier hasn't met supplier number requirements
- Not-contract supplier provides an item listed in a competitive bidding area
- Casher wants the detail or service before the advance coverage determination
We may hold you financially liable if you don't requite the beneficiary an ABN for 1 of these specific situations.
Don't use an ABN for Medicare Advantage (Part C) items and services or the Medicare Prescription Drug Benefit (Part D).
Y'all don't need to notify the beneficiary before you provide items or services that aren't a benefit or never covered. Section 20.2 of the Medicare Claims Processing Transmission, Chapter thirty has a list of Medicare non-covered items and services.
We recommend you effect a voluntary ABN or a similar discover equally a courtesy to alert the beneficiary nigh their fiscal liability.
An ABN is valid if you:
- Use our most recent version approved by the Office of Management and Upkeep (OMB)
- Use a single ABN for an extended form of treatment for no longer than one yr
- Complete the entire class
- Ensure the beneficiary understands the detect
What if the Beneficiary or their Representative Refuses to Cull an Selection or Sign the ABN?
If the beneficiary or their representative refuses to choose an option or sign the ABN, y'all should note that on the original ABN. You may list refusal witnesses, but it'due south not required. If a beneficiary refuses to sign a correctly issued ABN, consider not providing the detail or service unless the consequences (health and safety of the casher or ceremonious liability in case of harm) prevent it.
Close
ABN Tutorial
In this ABN tutorial, select whatever field (letters A–J) for details on how to complete each ABN section.
Entities who issue ABNs are collectively known equally "notifiers." Notifiers can include physicians, practitioners, providers (including labs) and suppliers, and utilization review committees.
If you reproduce the ABN, remove the letters before issuing it to the casher.
Become to the ABN Tutorial
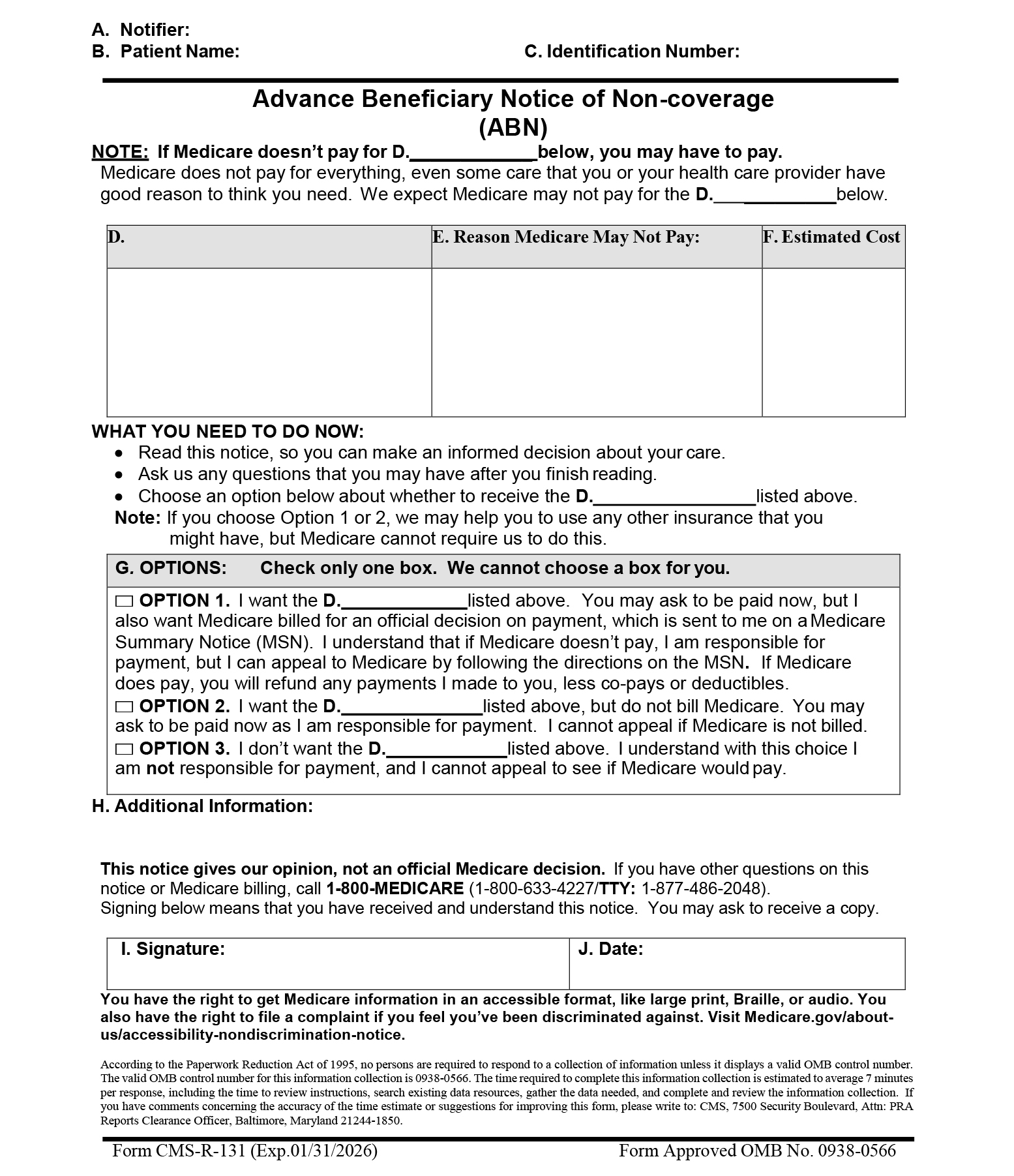
A. Notifier(s)
- Yous must place their name, accost, and phone number (including TTY number, when needed) at the peak of the observe. You may add this information to your logo at the summit of the notice past typing, hand-writing, pre-printing, using a characterization, or other means.
- If you and the billing entity aren't the same, you may listing more than than ane entity in the Header if it's specified in the Boosted Information (H) section who we should contact with billing questions.
B. Patient Name
- You lot must enter the beneficiary's start and last name and include a middle initial if it appears on their Medicare menu. Nosotros won't invalidate the ABN because of a misspelling or missing initial if the casher or representative recognizes the name listed on the detect every bit the casher's.
C. Identification Number
- This field is optional. If in that location'due south no identification number, it doesn't invalidate the ABN. You may enter a beneficiary identification number that links the notice with a related claim, and you may create an internal filing number, like a medical tape number. Don't listing Medicare Casher Identifiers (MBIs) or SSNs on the notice.
First ABN D. Field
List 1 of these descriptors:
- Item
- Service
- Lab test
- Test
- Procedure
- Care
- Equipment
2d ABN D. Field
Use the same wording used in the outset (D) field.
Third ABN D. Field
Use the same wording used in the outset (D) field.
Offset D. Column
- The notifier must list the specific items or services they believe nosotros won't cover in the blank (D) column
- In a fractional denial case, you must list the item's or service'due south backlog component(south) for which deprival is expected in the blank (D) column.
- Put general descriptions of specifically grouped supplies in this column. For example, wound care supplies is plenty to describe an detail group. We generally don't require an itemized listing of each supply.
- When yous reduce a service, you must provide enough information so the casher understands why. For case, we consider wound care supplies decreased from weekly to monthly plenty to draw a frequency subtract for this supply category; just writing wound care supplies decreased isn't enough.
- Yous must complete all 7 blank (D) fields to validate the notice. We encourage you lot to populate all blank (D) fields earlier using a general descriptor like Item(s) or Service(southward).
E. Reason Medicare May Not Pay
In this column, notifiers must explain, in casher friendly language, why they believe Medicare may not embrace the items or services in column (D). Three non-coverage reasons nosotros commonly apply:
- Nosotros don't pay for this test for your condition
- Nosotros don't pay for this examination this often (denied equally too frequent)
- Nosotros don't pay for experimental or inquiry tests
To be a valid ABN, you must list at to the lowest degree 1 reason for each detail or service in column (D). You tin can use the same non-coverage reason for multiple items in column (D) when advisable.
F. Estimated Cost
- Notifiers must consummate column (F) to ensure the beneficiary has all available information to make up one's mind whether to get potentially non-covered services.
- You must make a practiced faith effort to listing a reasonable dollar estimate for all items or services in column (D). Nosotros wait the guess be inside $100 or 25% of bodily costs, whichever is greater; generally, we accept estimates exceeding the bodily cost, since it won't harm the beneficiary if actual costs are less than predicted.
- Notifiers can parcel routinely grouped items or services into a single cost judge. For instance, you may give a single cost gauge for a group of lab tests like a Basic Metabolic Panel (BMP). We accept an average daily price judge for long-term or complex projections.
- You may also pre-impress a carte du jour of items or services in column (D) and include a price approximate abreast each item or service. If a state of affairs calls for additional tests or procedures (such equally lab reflex testing), and you tin't reasonably estimate those test costs at ABN delivery, you may enter the initial price estimate and betoken possible farther testing.
- If you lot can't provide a good organized religion projected cost approximate at ABN delivery, you lot may signal in the cost approximate expanse there's no cost estimate available. You shouldn't employ these terminal 2 scenarios routinely or frequently, merely the beneficiary has the option of signing the ABN and accepting liability in these situations.
M. Options
Complete the iii (D) fields under the (Thousand) Options department with the same wording used in the outset (D) field. The beneficiary, or their representative, must choose i of the 3 options listed. We don't allow you to make this option.
Special guidance for people who are dually enrolled in both Medicare and Medicaid, also known as dually eligible individuals (has a Qualified Medicare Casher [QMB] Program and or Medicaid coverage), ONLY:
Instruct them to check ABN Choice Box 1 and so the notifier tin can submit the merits for Medicare adjudication. Strike through Option Box one language as shown here:
□ OPTION 1. I want the D._______ listed above. Yous may inquire to be paid now, but I too want Medicare billed for an official decision on payment, which is sent to me on a Medicare Summary Find (MSN). I understand that if Medicare doesn't pay, I am responsible for payment, but I can entreatment to Medicare past following the directions on the MSN.
Nosotros require these edits because the notifier can't bill the dually eligible beneficiary when they offer an ABN. Y'all must not bill the beneficiary pending Medicare and Medicaid adjudication, because federal police affects dually eligible casher coverage and billing.
If we deny a claim when you needed an ABN to transfer financial liability to the beneficiary, cantankerous the claim over to Medicaid or submit it for arbitrament based on state Medicaid coverage and payment policy. Medicaid will issue a Remittance Advice based on this determination. Once Medicare and Medicaid adjudicate the claim, you may only charge the patient in these circumstances:
- If the beneficiary has QMB coverage without full Medicaid coverage, the ABN could allow you to shift financial liability to the beneficiary per Medicare policy
- If the beneficiary has full Medicaid coverage and Medicaid denies the merits (or won't pay considering you don't participate in Medicaid), the ABN could permit y'all to shift financial liability to the beneficiary per Medicare policy, bailiwick to land laws that limit beneficiary liability
Note: The beneficiary doesn't demand to check an choice box or sign and appointment the notice when yous issue the ABN as a voluntary notice.
Selection 1
The casher wants to go the items or services listed and accepts fiscal responsibility if we don't pay. They agree to pay now, if required. Notifiers must submit a claim to Medicare that results in a payment decision the casher can appeal. If they demand a Medicare claim denial for secondary insurance to cover the service, y'all may advise them to select Option 1.
Special guidance for non-participating suppliers and providers (those who don't accept Medicare consignment) Just:
Strike the last Option Box i sentence as shown here:
□ Pick 1. I desire the D. ___________ listed above. Y'all may enquire for payment now, only I also want Medicare billed for an official conclusion on payment, sent to me, on a Medicare Summary Discover (MSN). I understand if Medicare doesn't pay, I am responsible for payment, only I can appeal to Medicare by post-obit the MSN directions. If Medicare does pay, you will refund any payments I made to you, less co-pays or deductibles.
Notifiers, include this single line strike on ABNs printed specifically when you provide unassigned items and services. You can also hand-pen the line on an already-printed ABN. Don't entirely muffle or delete the sentence. We don't require you or beneficiaries to initial abreast the sentence or date the annotations when you make the changes.
When y'all strike this judgement, you lot should include this CMS-canonical unassigned claim statement in the (H) Additional Data department:
"This supplier doesn't take Medicare payment for the item(south) listed in the table above. If I checked Pick ane above, I am responsible for directly paying the supplier's charge for the item(s). If Medicare does pay, Medicare will pay me the Medicare-approved corporeality for the item(due south), and this payment may be less than the supplier's charge."
You can include this statement on ABNs printed for unassigned items and services, or manus-write it in a legible 10 point or larger font.
Fourth ABN D. Field
Utilise the aforementioned wording used in the first (D) field.
Fifth ABN D. Field
Use the same diction used in the first (D) field.
Sixth ABN D. Field
Apply the same wording used in the beginning (D) field.
Option ii
The beneficiary wants to go the item or services listed and accepts financial responsibility. They agree to pay now, if required. When the casher chooses this option, y'all don't file a claim, and there are no entreatment rights.
You won't violate mandatory claims submission rules under section 1848 of the Social Security Act when you don't submit a claim at the beneficiary's written request.
Pick 3
The beneficiary doesn't want the intendance in question and you lot tin can't charge them for items or services listed. Yous don't file a merits, and there's no appeal correct.
H. Additional Information
Notifiers may use this space to clarify what they believe is useful to beneficiaries. You may employ this space to include:
- Statement advising the casher to notify their provider about sure ordered, but not received tests
- Information on other beneficiary insurance coverage, like a Medigap policy
- An additional dated witness signature
- Other necessary annotations
We assume notifiers fabricated annotations on the same date that appears in field (J), accompanying the signature. If they made the annotations on different dates, make those dates part of the annotations.
I. Signature
The casher (or representative) must sign the notice to indicate they got the detect and sympathize its contents. If a representative signs for a beneficiary, they should write out representative in parentheses after their signature. The representative'southward name should be clearly legible or noted in print.
J. Date
The beneficiary (or representative) must write the date they signed the ABN. If the beneficiary has physical difficulty writing and requests help completing this field, the notifier may write the date.
Resources
- Beneficiary Notices Initiative (BNI)
- BNI Mailbox
- Medicare Advance Written Notices of Non-coverage
- Department 50 of Medicare Claims Processing Manual, Chapter 30
Disclaimers
Medicare Learning Network® Content Disclaimer, Product Disclaimer, and Department of Wellness & Human Services Disclosure
This educational product was collaboratively developed by the Medicare Learning Network® (MLN) and Noridian Healthcare Solutions, LLC, to provide nationally consequent education on topics of interest to the health intendance professional community.
The Medicare Learning Network®, MLN Connects®, and MLN Matters® are registered trademarks of the U.S. Department of Wellness & Human Services (HHS).
Source: https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/ABN-Tutorial/formCMSR131tutorial111915f.html
Posted by: christiankeent1945.blogspot.com


0 Response to "When Are Providers Responsible For Obtaining An Abn For A Service Not Considered Medically Necessary"
Post a Comment